Rheumatoid arthritis (RA) is a chronic systemic inflammatory autoimmune disorder characterized by deforming symmetrical polyarthritis of varying extent and severity. It is associated with synovitis of joint and tendon sheaths, articular cartilage loss, erosion of juxta-articular bone, and the presence of IgM rheumatoid factor in the blood in most patients.1 In some patients, systemic and extra-articular features may be observed during the disease and rarely before the joint disease. These include anaemia, weight loss, vasculitis, serositis, interstitial inflammation in lungs and exocrine, salivary, and lacrimal glands, as well as nodules in subcutaneous, pulmonary, and scleral tissues.2

RA is the most common inflammatory arthritis, affecting approximately 0.1-2%
of the adult population worldwide. It is responsible for around 250,000
hospitalizations and 9 million physician visits every year. The onset of RA
usually occurs between 30 to 50 years of age and is 2-3 times more likely to
occur in women than men.3 In India, studies have confirmed the
prevalence rate to be between 0.28- 0.7%.4 Leti untreated,
about 20-30% of RA patients become permanently work-disabled within 3-4 years
of diagnosis. One of the forecasts suggests that the rate of
practioner-diagnosed arthritis will increase by almost 49% by 2040 due to the
worldwide ageing population.Genetic and environmental factors play a major role
in the development and progression of RA. Almost 55-60% of RA is from genetic
factors. Around 60 genetic loci exist associated with susceptibility of RA
across multiple populations.5 Changes in the synovial fluid of
patients with RA seem to increase the pro-inflammatory cytokines. Other factors
may include lifestyle choices, diet preferences, age, sex, and toxic exposures
that trigger the onset or progression of the disease.6
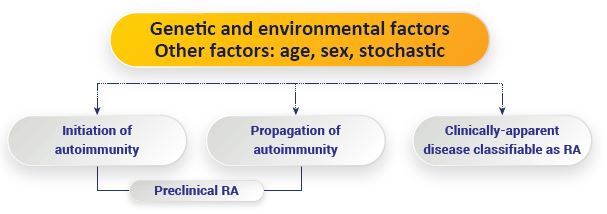
A major advance in how factors influence the development of RA, especially
seropositive RA, often involves increased production of antibodies that are
detectable more than 5-10 years before RA can be diagnosed. This period can be
termed as the ‘Preclinical Phase.’ In one study of patients with
musculoskeletal complaints, patients with the highest levels of antibodies at
baseline were at a 62% increased likelihood to be diagnosed with RA at five
years.7

Currently, two concepts predominantly guide early RA treatment.
1. Aggressive therapy
2. Treat to Target therapy
Early aggressive therapy uses medications to reduce inflammation and prevent
joint destruction that may lead to pain and disability. Treat to target therapy
is focused on treating the target i.e., the disease activity.8
The first-line therapy for RA treatment includes the use of NSAIDs and
corticosteroids. Fast-acting NSAIDs inhibit cyclooxygenase from preventing
prostaglandins, prostacyclin, and thromboxane synthesis. On the other hand,
corticosteroids are more potent, anti-inflammatory agents that prevent the
release of phospholipids and decrease the effects of eosinophils, thereby
reducing inflammation. The drawback of using these agents, however, is their
side-effect profiles.9
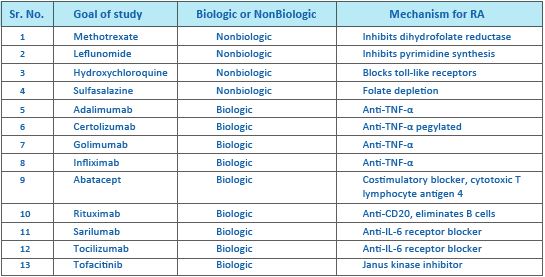
The second-line therapy for RA includes the Disease-modifying anti-rheumatic
drugs (DMARDs) that promote remission or slow/stop the progression of joint
destruction and deformity. These agents have been shown to reduce the risk of
developing lymphoma associated with RA. Methotrexate (MTX) is the first-choice
second-line drug. It is an immunosuppressive and analogue of folic acid that
impairs the metabolism of purines and pyrimidines and blocks the synthesis of
amino acids and polyamines.10
Joint surgery in patients with RA is usually the last resort for the
treatment of RA. The goal of surgical procedures in the management of RA is
primarily to reduce joint pain and restore the functions of the joints and
improve quality of life.
A wide range of non-pharmacologic treatment and management options are
available in the current day and age. The aim is to improve and amplify joint
movement, muscle strength, the performance of day-to-day activities with ease,
and to improve the quality of life (QOL) of patients suffering due to RA. These
treatment options also help reduce the impact of the disease and related
comorbidities. Patient education and counselling are central to the
management of RA.

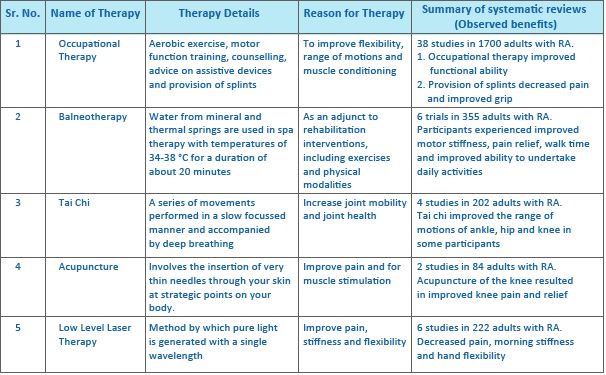
Other non-pharmacologic therapies include thermotherapy to improve stiffness
and relieve pain, joint protection, and energy conservation techniques like
aids, devices, and adaptations to the physical environment, use of orthoses
underpinned to a patient’s body to align, support, and improve function.
Special shoes and inserts are also used to reduce shock and provide further
support. Cognitive behavioural therapies are also developed to target the mood
of the patient’s suffering due to RA. It is a structured self-management
intervention that teaches a blend of cognitive and behavioural management.12
Omega-3 fatty acids may be protective and reduce the risk of RA.13 A
healthy eating pattern that includes whole grains, fruits, and vegetables has
also been correlated with a decreased diagnosis. Curcumin has also been
suggested as a supplement that may not only reduce inflammation in RA patients
but may also help manage the P. gingivalis infection seen in so many
of these patients.14
Rheumatoid arthritis is a disease that affects many people and has a
debilitating effect on the quality of life. New advances in rheumatoid
arthritis treatment are constantly being made. Both pharmacological, and
non-pharmacological therapies have shown to be effective in the treatment and
management of rheumatoid arthritis.
References: