Gastrointestinal discomfort is a very common complaint in pregnancy. In fact, most pregnant women will experience at least one GI discomfort like nausea, vomiting, GERD, etc., throughout their pregnancy.
While these conditions do occur in men and non-pregnant women, they occur more frequently during pregnancy because of the anatomic and physiologic changes associated with gestation. It is also difficult to manage GI issues in pregnant women because the effects of medications and other treatments on the developing fetus are often not extensively studied or are contraindicated. While these issues are rarely life-threatening, they can cause significant distress and impair the quality of life of the pregnant woman.

Some commonly encountered GI issues in Pregnancy are -
Hyperemesis Gravidarum
Nausea and vomiting in pregnancy is a very common condition that affects as
many as 70% of pregnant women. Although no consensus definition is available
for hyperemesis gravidarum, it is typically referred to as the severe form of
nausea and vomiting in pregnancy and has been reported to occur in 0.3–10.8% of
pregnant women. It is characterized by a triad of dehydration,
electrolyte imbalance, and more than 5% of weight loss from the pre-
pregnancy level, that accompanies severe nausea and vomiting.1
The Federation of Obstetric and Gynaecological Societies of India (FOGSI)
recommends a detailed history and examination to check for the female’s general
condition, vital signs, and signs of dehydration. Investigations like
urinalysis, complete blood counts and serum electrolytes are to be done to rule
out other causes, when symptoms are more severe. Whereas, the most severe cases
might require liver function tests, USG, blood sugar test, etc to offer
definitive management.
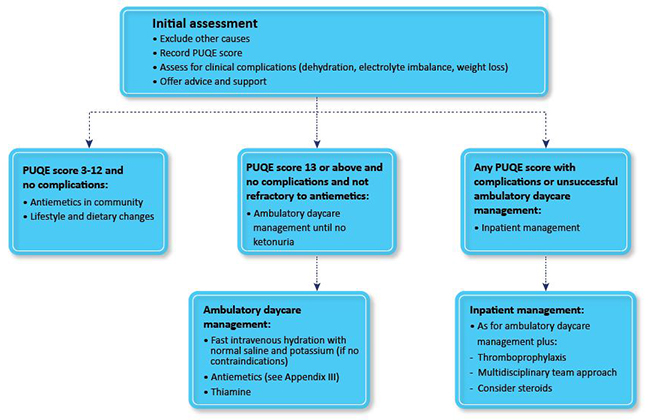
Another important parameter to assess is the PUQE score, which essentially
drives the management algorithms. The PUQE score stands for
Pregnancy-Unique Quantification of Emesis and Nausea and consists of a few
questions that objectively evaluate a patient’s symptoms.
Based on the PUQE score, the approach to females with Hyperemesis
Gravidarum is guided as follows2-
Constipation is yet another common complaint in pregnancy. Its symptoms may
include infrequent defecation, hard or scybalous stool, or excessive
straining. An extensive evaluation is usually unnecessary for women who
present with constipation for the first time during pregnancy.
The prevalence of constipation is estimated at 40% in pregnant women,
coming second after the most commonly occurring nausea and vomiting.3
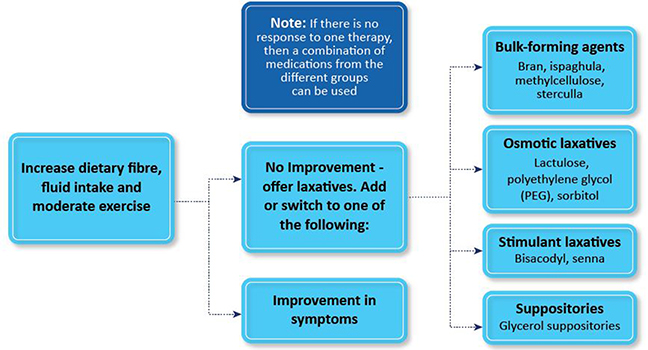
The majority of these females will find relief after diet modification and the
inclusion of more fibers.
Occasionally, pharmacological interventions may be required which include4
● Bulk-forming laxatives
● Osmotic laxatives
● Stimulant Laxatives
● Suppositories
About 30% of pregnant women have reported having GERD, particularly in the
second and third trimesters of their pregnancies. It is likely caused by a
reduction in lower esophageal sphincter pressure due to an increase in maternal
estrogen and progesterone during pregnancy.5 Hormonal changes in
pregnancy can also decrease gastric motility, resulting in prolonged gastric
emptying time and an increased risk of GERD.6
The management of GERD in the second and third trimester as per World
Gastroenterology Organisation guidelines includes7
● Lifestyle modifications, e.g., head-up position and avoiding heavy meals,
especially at night, may help relieve GERD symptoms associated with pregnancy.
● H2RAs, have been studied extensively and have a well-established efficacy and
safety in pregnancy.
● The US FDA has labeled all PPIs as Class B drugs (animal studies show no
risks, no human studies done), except for Omeprazole (Class C).
● It is important to engage the pregnant patient in a candid discussion
regarding the risks and benefits of PPI intake before prescribing these
medications.
Although IBD is mostly considered a chronic disease, it is said to be
present in about 0.67% of the pregnancies.8 The symptoms may
aggravate during pregnancy owing to the added pressure on the GI system. It is
also observed that fertility of women with active IBD is decreased.
Preconception counselling is advised for better outcomes in such cases.9
The line of treatment for pregnant women with IBD is same as non-pregnant
patients, as these drugs are considered safe except for some immunosuppressants
(e.g.methotrexate (MTX), mycophenolate mofetil, thalidomide). But, coordination
between obstetrician with a gastroenterologist is necessary while planning the
mode of delivery.10
The risk of developing gall stones increases during pregnancy owing to the
delayed emptying of the gall bladder due to hormonal changes. About 8% of
pregnant women have a tendency to form new gallstones by the third trimester,
but only about 1% have symptoms. Out of those with symptoms, less than 10%
develop complications. Most pregnant patients with gallstones are asymptomatic
and do not require further evaluation or treatment. For the more severe cases,
early diagnosis and cholecystectomy is shown to have good outcomes.11
Owing to the extreme hormonal and physical changes occurring during
pregnancy, gastrointestinal issues like nausea, vomiting, constipation are
extremely common. Moreover, untimely craving for different foods and
excessively controlled diet and appetite also exert an influence on the
female’s GI system. Chronic gastrointestinal diseases like GERD or IBD may pose
a therapeutic dilemma during pregnancy owing to the safety issues of
available drugs.
Dietary and lifestyle modification usually help with lesser severe symptoms,
whereas careful examinations and thorough investigations might be required to
come up with a management plan for a more severe set of issues, keeping in mind
the limited choice of drugs that are safe for the foetus.
References:
1. Fejzo, M.S., Trovik, J., Grooten, I.J. et
al. Nausea and vomiting of pregnancy and hyperemesis gravidarum. Nat Rev Dis
Primers 5, 62 (2019). https://doi.org/10.1038/s41572-019-0110-3
2.
https://www.fogsi.org/wp-content/uploads/committee-2020-activities/endocrinology-committee-vol-15-newsletter.pdf
3. Kuronen, Moona, et al. "Pregnancy, puerperium and perinatal
constipation–an observational hybrid survey on pregnant and postpartum women
and their age‐matched non‐pregnant controls." BJOG: An International
Journal of Obstetrics & Gynaecology 128.6 (2021): 1057-1064.
4. Verghese, TS, Futaba, K, Latthe, P. Constipation in pregnancy. The
Obstetrician & Gynaecologist 2015; 17:111– 5.
5. Fill Malfertheiner, S., Malfertheiner, M.V., Kropf, S. et al. A prospective
longitudinal cohort study: evolution of GERD symptoms during the course of
pregnancy. BMC Gastroenterol 12, 131 (2012). https://doi.org/10.1186/1471-230X-12-131
6. Ali, Raja Affendi Raja, and Laurence J. Egan. "Gastroesophageal reflux
disease in pregnancy." Best Practice & Research Clinical
Gastroenterology 21.5 (2007): 793-806.
7. Hunt, Richard, et al. "World gastroenterology organisation global
guidelines: GERD global perspective on gastroesophageal reflux disease."
Journal of clinical gastroenterology 51.6 (2017): 467-478.
8. Jølving, Line Riis, et al. "Prevalence of maternal chronic diseases
during pregnancy–a nationwide population based study from 1989 to 2013."
Acta obstetricia et gynecologica Scandinavica 95.11 (2016): 1295-1304.
9. Winter, R.W., Friedman, S. Update on Pregnancy in Patients with IBD. Curr
Treat Options Gastro 18, 423–441(2020). https://doi.org/10.1007/s11938-020-00303-0
10. Szymanska E, Kisielewski R, Kierku ´ s J, Reproduction and ´ Pregnancy in
Inflammatory Bowel Disease -Management and Treatment Based on Current
Guidelines, Journal of Gynecology Obstetrics and Human Reproduction
(2020), doi: https://doi.org/10.1016/j.jogoh.2020.101777
11. Celaj S, Kourkoumpetis T. Gallstones in Pregnancy. JAMA. 2021;325(23):2410.
doi:10.1001/jama.2021.4502